We are born with all the eggs we’ll ever have
What is ovarian reserve testing?
Put simply, ovarian reserve testing is an effective way of predicting how well your body may respond to fertility treatment by estimating the number and quality of eggs remaining in your ovaries. It helps assess:
- Egg quantity
- Egg quality
- Fertility potential
- Ideal timing for family planning
- Need for fertility support
Ultimately, ovarian reserve testing gives your fertility specialist a clearer picture of your reproductive potential and can help guide important decisions about family planning, fertility preservation, or treatment strategies.
Who should get ovarian reserve testing?
Ovarian reserve testing is generally recommended if you:
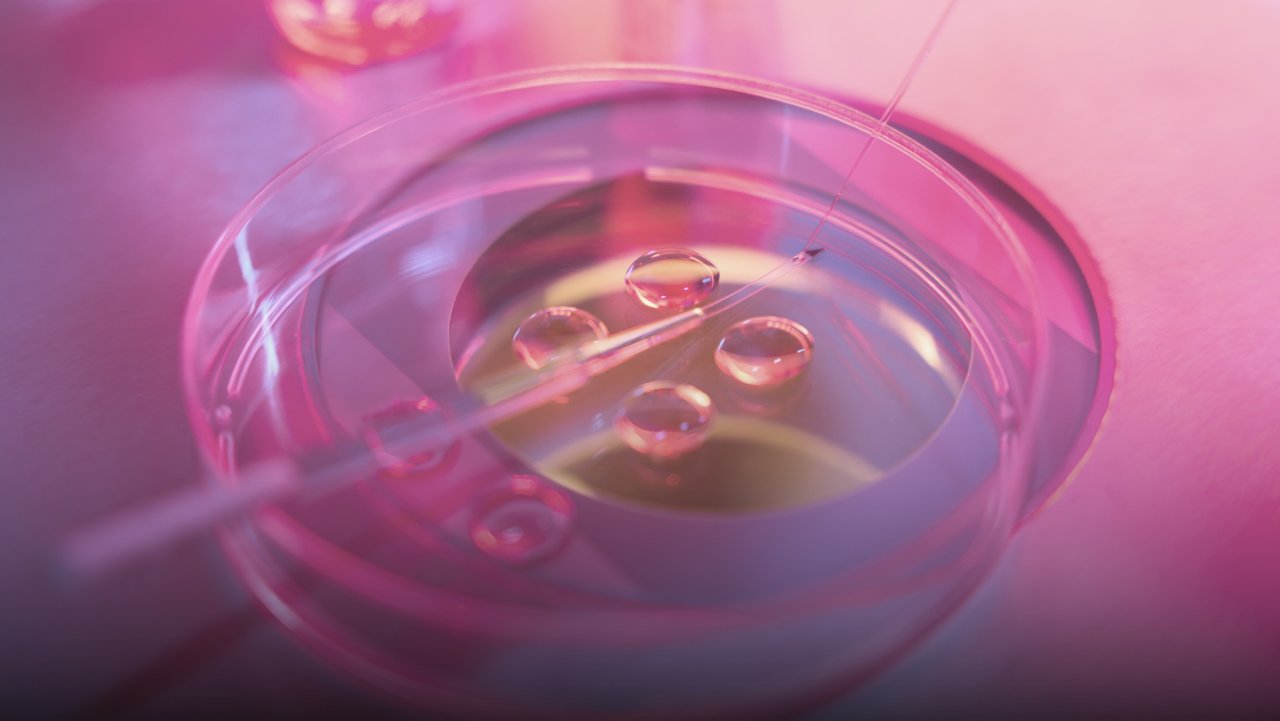
- Are considering assisted reproductive technologies, such as in-vitro fertilisation (IVF) or egg freezing
- Are over the age of 35 and are looking to get pregnant
- Have been trying to conceive for over 6 months to a year
- Are experienced chemotherapy, radiation or surgery
- Have a family history of fertility issues or early menopause
- Experience irregular periods
- Have gynaecological conditions, such as PCOS or endometriosis
That being said, you may even opt to check your ovarian reserve simply to stay informed and plan ahead. Even if you’re not trying to conceive right now, having a clear picture of your fertility can help you make confident, future-focused decisions on your own terms.
Types of ovarian reserve tests
Ovarian reserve testing can include one or more of the following tests:
- Anti-müllerian hormone (AMH) test — This is a baseline blood test that measures levels of AMH, a hormone produced by cells in ovarian follicles. Higher AMH levels indicate a greater ovarian reserve, while lower levels may suggest a lower quantity of eggs.
- Antral follicle count (AFC) — An AFC is performed by your gynaecologist via transvaginal ultrasound. This allows your doctor to identify the number of antral follicles (fluid-filled sacs that contain immature eggs) in the ovaries at the beginning of a menstrual cycle. Ultimately, the total count of antral follicles reflects the number of eggs potentially available for ovulation.
- Follicle-stimulating hormone (FSH) test — This blood test is generally performed on the 2nd or 3rd day of your menstrual cycle. FSH levels provide insight on how much stimulation the brain needs to get the ovaries to produce eggs. Higher FSH levels may mean reduced ovarian responsiveness and a lower egg supply.
- Estradiol (E2) test — This blood test can be done together with FSH test, at the 2nd or 3rd day of your menstrual cycle. Estradiol is a form of oestrogen produced by the ovaries. Abnormally high levels of estradiol can suppress FSH, which can lead to a poor ovarian reserve.
Factors that can affect your ovarian reserve test results
A variety of factors can affect your ovarian reserve test results, such as age, genetics, certain medical conditions, or even certain medications.
- Age — Our ovarian reserve naturally declines with age (especially after 35), and is the most significant factor that affects ovarian reserve test results.
- Medical conditions — Reproductive-related conditions, such as early menopause, endometriosis, or autoimmune disorders, can lead to a lower ovarian reserve.
- Previous ovarian surgery — Previous surgeries involving the ovaries, such as a cystectomy or tubal surgeries, can lower ovarian reserve.
- Cancer treatments — Cancer therapies, such as chemotherapy or radiation can negatively affect egg quality.
- Lifestyle factors — Smoking, excessive alcohol and chronic stress can negatively affect hormone levels which, in turn, affect one’s ovarian reserve
- Medications — Certain medications can influence your ovarian reserve test results
- Body weight — Extremely low or high body weight can affect your ovarian reserve. Being extremely underweight can lead to irregular or absent ovulation, while obesity is often associated with insulin resistance or high androgen levels, affecting hormone regulation.
- Hormonal imbalances — Hormonal imbalances, such as PCOS, may lead to high ovarian reserve results, but ovulation may be irregular and egg quality may be compromised.
There are also temporary factors that can affect ovarian test results, such as:
- Hormonal contraceptives — Birth control medication can suppress natural hormone fluctuations and ovulation. This leads to temporarily low levels of FSH or AMH hormones, or even reduce the number of follicles seen during an ultrasound.
- Recent illness or stress — Illness or stress can temporarily affect hormone production.
- Medications — Certain medications, such as steroids, can cause hormonal imbalances and create inconclusive test results.
- Timing of the menstrual cycle — Certain ovarian reserve tests need to be done on day 2 or 3 of your cycle, otherwise, the results will not accurately reflect your true ovarian function.
Can you improve your ovarian reserve?
Unfortunately, there we are born with all the eggs we’ll ever have, and this number naturally declines as we age. However, there are steps you can take to protect the eggs you currently have and to improve their quality.
- Freeze your eggs early — As the quality of your eggs decline as you age, freezing them early (in your 20’s to 30’s) will preserve the eggs at a healthier state. These can be used later in assisted reproductive technologies for higher pregnancy success rates later on in life.
- Quit smoking — Quit smoking to prevent affecting ovarian function.
- Maintain a healthy lifestyle — Having a diet rich in antioxidants and exercising moderately can help support a healthy ovarian reserve.
- Avoid alcohol — Alcohol can disrupt reproductive hormones and may lower anti-müllerian hormones, which negatively affect ovarian reserve health and compromise egg quality.
Summary
Ovarian reserve testing is an important first step to understanding your fertility. Our ovarian reserve naturally declines with age, but it can be improved — especially if you’re planning for a family now, or in the future.
Dr Tan believes that xx. Schedule a consultation with us today for a proper diagnosis and personalised treatment plan to optimise your ovarian health.
Frequently Asked Questions
Do I need to stop birth control before going for an ovarian reserve test?
In some ovarian reserve tests, such as FSH, LH and Estradiol tests, you may be required to stop your hormonal contraceptives a month or more before testing. During your consultation, be sure to let your fertility specialist know, so that they can advise you on what you need to do to prepare for your ovarian reserve test.
Is ovarian reserve testing painful?
No, ovarian reserve testing is well-tolerated. It generally requires a blood draw and a transvaginal ultrasound.
What do low ovarian reserve results mean?
Low ovarian reserve results don’t necessarily mean you can’t conceive. It simply means you may have a shorter reproductive window and require timely fertility planning or medical support.
Should I freeze my eggs if I have a low ovarian reserve?
Egg freezing may be a proactive measure for preserving your fertility if you have a low ovarian reserve. Your fertility specialist will advise you on whether this is a good option to consider.