What is Conventional IVF?
Conventional IVF is a fertility treatment that involves stimulating the ovaries with hormonal medication to produce multiple eggs. These are then retrieved, fertilised in a lab (with your partner’s sperm), and transferred back into the uterus once ready.
This helps increase your chances of a successful pregnancy by creating more embryos in a single cycle.
Conventional IVF process — What to expect
A conventional IVF journey is a time-sensitive process that requires both commitment and emotional resilience. Rest assured, your IVF doctor will work closely with you and guide you every step of the way.
- The use of ICSI (for male factor infertility)
The ovaries are stimulated with hormonal injections to produce multiple mature eggs. This is done for a period of 8 to 14 days. Follicle development and hormone levels are then monitored via regular ultrasounds and blood tests. - The use of ICSI (for male factor infertility)
The ovaries are stimulated with hormonal injections to produce multiple mature eggs. This is done for a period of 8 to 14 days. Follicle development and hormone levels are then monitored via regular ultrasounds and blood tests. - Egg retrieval (34-36 hours post-trigger)
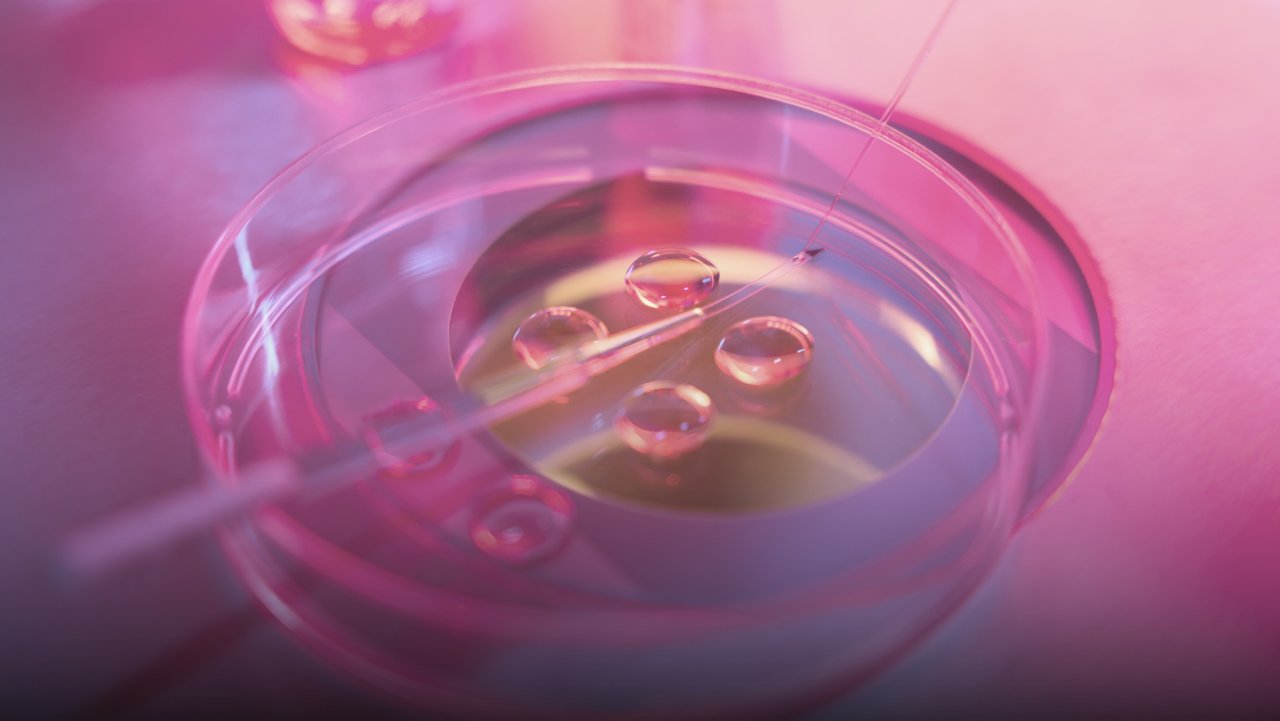
Also known as the “oocyte pick-up”, egg retrieval is a minor procedure performed under light sedation. A thin needle is passed through the vaginal wall to collect the eggs from the ovaries. This procedure is generally painless and you may go home within the same day. - Fertilisation & embryo culture (3-5 days post-retrieval)
The retrieved eggs are fertilised with your partner’s sperm in the lab. The embryos are then cultured and monitored for 3-5 days, and the best quality ones are selected for transfer or freezing. - Embryo transfer (day 3 or day 5)
A quality embryo is selected and transferred into the uterus using a thin catheter. You will be advised to rest briefly before returning home. - Luteal phase support (starts post-transfer)
Progesterone supplements are prescribed to support implantation and pregnancy. - Pregnancy test (10-24 days after embryo transfer)
A blood test will be taken to check for successful implantation. If positive, follow-up scans will be done to confirm a healthy pregnancy.
What is Mini IVF?
Mini IVF, also known as minimal stimulation IVF, is a gentler approach in comparison to conventional IVF. As its name suggests, it involves the use of lower-dose ovary-stimulating medication, such as oral medication like Clomid or low-dose injectable gonadotropins.
With mini IVF, there is more focus on egg quality over egg quantity, and is an ideal option for those who have a lower ovarian reserve and want a more natural, less invasive option. It is important to note that fewer eggs does equate to fewer embryos, hence lower success rates of pregnancy per cycle.
However, with the right patient, personalised treatment plan, and putting more focus on egg quality over egg quantity, it is still possible to achieve results.
| Factor | Mini IVF | Conventional IVF |
| Medication | Keyhole-sized, under 1cm | Larger incisions, typically 10-15cm |
| Egg retrieval | Fewer eggs (usually 3-5) | More eggs (usually 10-15 or more) |
| Cycle intensity | Gentler on the body | More aggressive approach |
| Cost per cycle | Typically lower | Higher due to cost of medication and lab work |
| Embryo freezing potential | Lower freezing potential as less embryos available | Higher chance of surplus embryos for freezing |
| Time to pregnancy | May require multiple cycles to achieve pregnancy | Higher success rates per cycle, with a chance of earlier pregnancy |
| Personalisation | More tailored to your individual needs | More standardised protocols |
| Success rates per cycle | Generally lower | Typically higher, as there are more eggs and embryos |
| Ideal for | Women with low ovarian reserves, older age, or a gentler approach IVF approach | Women with normal ovarian reserves who want higher success per cycle |
Which IVF approach is right for you?
There is no “best” approach when it comes to IVF, but rather one that best suits you. When it comes to choosing between a Mini IVF and Conventional IVF procedure, here are some factors to consider:
- Age — Age plays a crucial role in fertility treatment because with time, egg quality and quantity naturally decline. Mini IVF may be an ideal option for those in their late 30s or 40s, who want a gentler procedural approach, with less medication exposure while retrieving viable eggs. Younger patients may prefer Conventional IVF, especially if they would want to freeze some embryos for future family planning. The use of ICSI (for male factor infertility)
- Ovarian reserve — A low ovarian reserve may mean your body might not respond well to high stimulation, making Mini IVF a more ideal option. However, with a healthy reserve, opting for a Conventional IVF can maximise your egg retrieval and increase your chances of a successful fertilisation.
- Hormone sensitivity — If you are sensitive to fertility medication, and experience bloating, moodswings, or even ovarian hyperstimulation syndrome (OHSS), Mini IVF might be a better option for you as significantly lower hormone doses are prescribed.
- Desired number of embryos — If you intend to freeze your embryos for the future, then Conventional IVF is recommended. This procedure produces more eggs and more embryos.
- Time constraint — If you would like to achieve pregnancy at an earlier time, Conventional IVF offers a higher rate of success per cycle, which means fewer cycles required to achieve your pregnancy goal.
- Budget — A Mini IVF procedure typically costs less as it requires fewer medication and lesser monitoring, making it an ideal option if you’re looking to stretch your budget.
- Lifestyle and schedule — A Mini IVF procedure may be less taxing as it is lower in intensity, requiring fewer injections and less frequent clinic visits, making it an ideal option for those with a hectic schedule.
- Fertility history and diagnosis — Your reproductive history and health can make a big difference when it comes to choosing what type of IVF procedure to opt for. This can include a history of failed IVF cycles, PCOS, endometriosis, or other unexplained fertility issues.
Your gynaecologist’s recommendation
Choosing between a Mini IVF and Conventional IVF can be a daunting decision, with each procedure having their own pros and cons. Thankfully, you don’t have to make this decision on your own. Your IVF specialist will look at your lab results, scan findings and your medical history to recommend a personalised protocol that will help you achieve your desired results.
Here at Majella Women’s Specialist , Dr Tan Heng Hao and his clinical team are dedicated to supporting you through your unique fertility journey with expertise and personalised care.
Schedule a consultation with us today for a detailed diagnosis and personalised treatment plan.